Nosokinetics
Nosokinetics - Staking our claim
By Mark Mackay, University of Adelaide
(comments to rjtechne@iol.ie)
Introduction
The health system is complex! Well we all knew that. As people interested in modelling the health system, and in particular, modelling aspects to deal with patient flow, we often focus on just that - modelling patient flow. To get recognition of the value of this type of work we need more than just modelling skills and the ability to sell the skills. The purpose of this paper is to suggest some of the solution, but also hopefully create some debate about other possibilities.
Thereís Two Sides to the Health System Coin
We tend to be interested in the health demand issues, such as queue times and capacity planning. This probably stems from the drivers of our interests - bed blockages, political and media interests, funding interests etc. Also, thereís been much work in recent years to suggest that demand for services will increase. This, in part at least, is due to the fact that the number of older people in developed countries is about to increase and older people use more health care resources than younger people (in general). This is a well-established trend. Thus, there is a forecast increase in demand for services. Other drivers of increased demand include changes in technology and consumer expectations.BUT thereís a supply side to this industry as well and itís one thatís often overlooked. To fix the problem, whatever it may be, often involves adding more resources. In health more resources usually means more staff somewhere.
The changing population profiles have a double whammy effect - at the very time when there are more older people demanding services, the number of workers will decline (the baby boomers are retiring). This leads to a supply and demand forecast that looks something like the following schematic diagram.
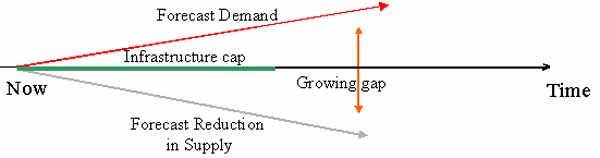
Figure 1: Supply and Demand Forecast.
We have increasing demand and decreasing supply. So far Iíve just been talking about the people in the system (the service providers and patients). Consequently, there is a gap between the expected demand and ability to supply the services.
Did I forget to mention that many hospitals are at capacity and this represents an infrastructure cap. Our ability to provide more services is limited by physical infrastructure. This, of course, can be overcome given time and resources - just build more buildings etc. However, it doesnít resolve the shortage of staff!
This is a global problem! The gap between supply and demand represents a problem and an opportunity. This is where those working on nosokinetics can help.
Stretching Capacity
It may seem obvious, but if many hospitals were computer networks or telephone service providers, theyíd be out of business. Why? Systems canít operate at near capacity for extended periods when variability exists. This is illustrated in the next diagram.
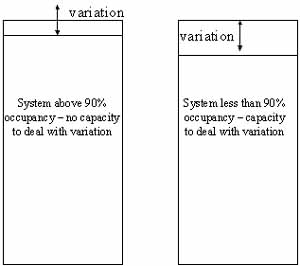
Figure 2: Variability Effects
This is probably one of the first points we should learn to make (apart from also emphasizing that the average length of stay is a poor measure of patient stay). This is particularly important where physical infrastructure gaps exist. Solving patient flow issues where variation in daily demand cannot be readily handled and future demand is expected to increase isnít likely to lead to long-term stable solutions. Donít get me wrong - there are gains are to be made, but itís a matter of whether these gains can provide both the capacity required to avoid constant crises and cope with increases in demand.
This leads nicely to the observation that there are perhaps several themes within the nosokinetics continuum, namely: the highly quantitative capacity planning, and efficiency and effectiveness work, but also the more qualitative or soft type work, such as trust - distrust relationship modelling (Kethers et al., 2005). The soft type work shouldnít be over looked, as the potential for good outcomes or returns on efforts exists.
The Source of the Solutions
We all know that there is much to be done in the health system. But who can provide the solutions? The following diagram attempts to show the players who can be a part of the health game.It should be acknowledged that those in the Nosokinetics group are likely to have interests in mathematics and statistics. Thus, there is both potential to grow those interested in Nosokinetics and also the role of nosokinetics in solving health care system problems!
Importantly, no-one group will own the solution. Rather, working across boundaries is the only way to get meaningful and accepted solutions.
Enhancing the likelihood of take-up
In a recent system dynamics list serve exchange on how to improve the take-up and acceptance of system dynamics, Jean-Jacques Laublť Allocar, a CEO in France, observed:- If you want to sit at their table you must understand their preoccupations
- Discuss with them at their own level of understanding using their language and not be boring.
- You must learn to sell yourself and not a method.
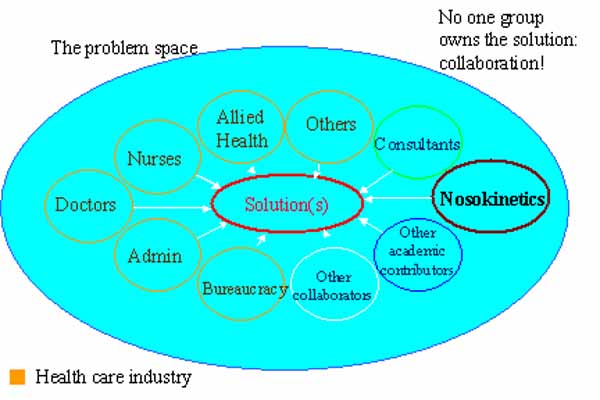
Figure 3: Factors Influencing Uptake Liklihood
These are all good points. I would go further and suggest that there are a range of solutions, some of which those interested in Nosokinetics can directly influence, for example do some work for a health care organisation, and others that are system solutions, for example changing curricula at universities so that those training to become health professionals are aware of the role of nosokinetics. The following diagram attempts to show some the solutions - note: no single solution will work.

Figure 4: Multiple Channels of Influence
Ensuring that we hang out our shingle that weíre here to do business is also helpful. We should be mindful that in doing so we aim to help solve the clientís problem rather than imposing our solutions on them, particularly when others may provide better solutions.
Conclusion
Itís important to remember that patient flow doesnít occur without two things: patients and service providers. We need to be mindful of both. Thereís no point in coming up with good work about patients if we ignore the plight of the workforce.Is the glass half-empty or half-full? If itís half-empty, letís give up now and go home or join another game. If the glass is half-full, then thereís plenty of opportunity to contribute to the health care sector. Itís not necessarily going to be easy going though - particularly as we all know itís not easy to get funding for health services or systems research type work - and it may take time.
Reference:
Kethers, S; Gans, G; Schmitz, D and Sier, D (2005). Modelling Trust Relationships In A Healthcare Network: Experiences With The Tcd Framework. 13th European Conference on Information Systems
Some navigational notes:
A highlighted number may bring up a footnote or a reference. A highlighted word hotlinks to another document (chapter, appendix, table of contents, whatever). In general, if you click on the 'Back' button it will bring to to the point of departure in the document from which you came.Copyright (c)Roy Johnston, Ray Millard, 2005, for e-version; content is author's copyright,